Services
Let's Talk
Services
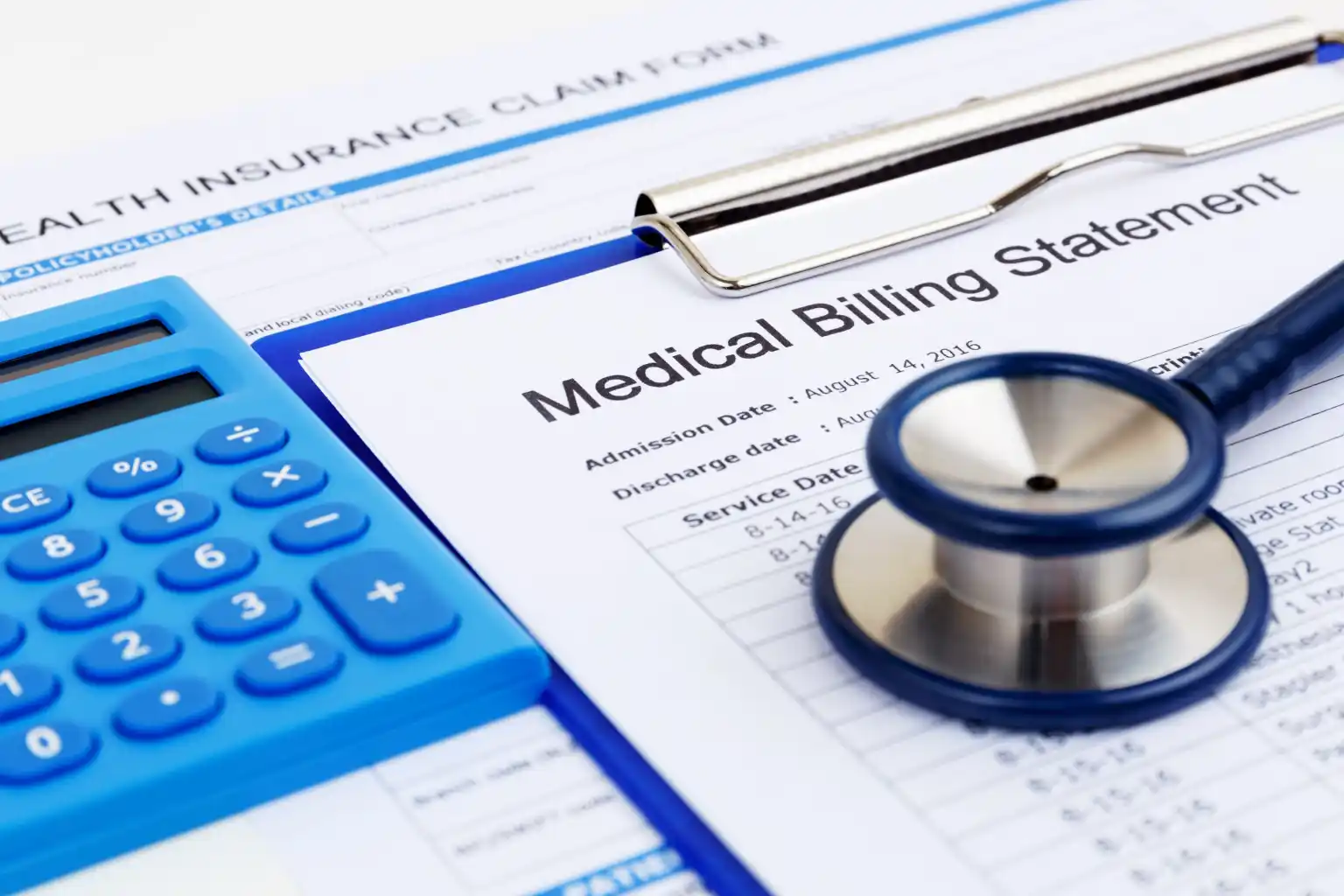
Streamlining
Revenue Cycle Management (RCM)
We offer end-to-end support across 10 essential back-office functions, ensuring your clinic runs like clockwork.

1. Patient Demography Capture
We accurately input and validate patient demographic information such as name, DOB, insurance details, contact info, and more — ensuring your system is always updated.
Why it matters:
- Incorrect patient data = delayed or denied claims
- With 99.8% accuracy, we reduce claim rejections due to errors in basic information
- Fewer data-entry errors
- Reduced rework for front-desk teams
- Faster patient onboarding
2. Appointment Scheduling
We manage your calendars across platforms like Zocdoc, eClinicalWorks, and RingCentral, handling new bookings, reschedules, cancellations, and automated reminders.
Why it matters:
- Missed or double-booked appointments = revenue loss
- Our 24/7 scheduling support reduces no-shows by up to 40%
Impact:
- Improved patient satisfaction
- Fully booked schedules
- Streamlined front-desk workflow


3. Eligibility Verification
We check patients’ insurance coverage before their visit — including plan validity, co-pays, deductibles, and benefits — through payer portals and clearinghouses.
Why it matters:
- Discovering non-coverage after treatment = unpaid claims
- Verifying before the visit ensures a smooth check-in and billing process
Impact:
- Increase clean claim rate
- Avoid treatment gaps due to insurance denials
- Save time for billing teams
4. Charge Posting
We post charges into your EMR/billing system from visit notes, ensuring all CPT/ICD-10 codes are captured accurately and tied to each patient encounter.
Why it matters:
- Delay or inaccuracy in charge posting = billing delays
- Our fast turnaround enables same-day or next-day billing
Impact:
- Immediate revenue recognition
- High coding accuracy
- Reduced denial rates


5. Electronic Claims Submission
We create, review, and submit claims electronically through clearinghouses, ensuring they’re properly formatted and submitted on time.
Why it matters:
- Claim errors = payment delays
- Our team ensures that claims are error-free and submitted promptly
Impact:
- 98%+ first-pass acceptance
- Quicker reimbursements (5–7 days)
- Less manual work for billing teams
6. Claim Scrubbing
We thoroughly review and clean up claims before submission — checking for missing modifiers, incorrect coding, or NPI mismatches.
Why it matters:
- A single coding error can get a claim denied
- Pre-submission scrubbing avoids delays and rework
Impact:
- Up to 95% clean claims
- Higher approval rates on first submission
- Better compliance

7. Payment Posting
We process Electronic Remittance Advice (ERA) and Explanation of Benefits (EOB) to update payment records quickly and accurately in your system.
Why it matters:
- Delayed posting = outdated revenue reports and errors in AR
- We ensure payments, adjustments, and write-offs are correctly logged
Impact:
- Real-time visibility into revenue
- Identifies underpayments or denials quickly
- Helps close monthly books faster
8. Accounts Receivable (AR) Follow-Up
We follow up on unpaid claims with insurance providers, identifying reasons for delay or non-payment, and work to resolve them promptly.
Why it matters:
- Old claims = lost revenue
- Consistent AR follow-up keeps your cash flow healthy
Impact:
- Reduce aging AR >90 days
- Improve collection rates
- Fewer write-offs


9. Denial Management
We analyse claim denials, correct the root cause (coding, eligibility, submission error), and resubmit them within payer deadlines.
Why it matters:
- Denials impact your bottom line
- Without a clear process, you lose revenue you’ve already earned
Impact:
- Recover revenue from denied claims
- Improve long-term clean claim performance
- Learn from trends to prevent future denials
10. Patient Statements
We generate and send clear, timely billing statements to patients via print or digital methods, including payment support (phone/email).
Why it matters:
- Unclear or delayed statements = unpaid bills
- Our friendly approach improves collection without hurting patient relationships
Impact:
- 20–30% better patient payment rates
- Fewer billing disputes
- Improved patient trust