Empowering Healthcare, Beyond Boundaries
Outsource Smarter. Operate Smoother. Care Better.
Your trusted partner in healthcare back-office support – delivering faster workflows, lower costs, and higher accuracy to clinics across the U.S.
Make an Enquiry
Let’s Talk
About Us
Smart Back-Office Solutions for Healthcare Clinics
Cut costs, boost accuracy, and streamline operations—trusted support across the U.S.
At MedAxis Global, we’re more than a service provider — we’re an extension of your team. Based in India, we help clinics in the U.S. simplify and optimize their administrative workflows so they can focus on what matters most: patient care.


Why MedAxis Global?
- 40–60% cost savings compared to in-house teams
- 99.5%+ data accuracy across all services
- 24–48 hours turnaround time
- HIPAA-compliant, secure infrastructure
- Trusted by leading clinics
Services
Streamlining
Revenue Cycle Management (RCM)
We offer end-to-end support across 10 essential back-office functions, ensuring your clinic runs like clockwork.

Patient Demography Capture
We accurately input and validate patient demographic information such as name, DOB, insurance details, contact info, and more — ensuring your system is always updated.

Appointment Scheduling
We manage your calendars across platforms like Zocdoc, eClinicalWorks, and RingCentral, handling new bookings, reschedules, cancellations, and automated reminders.

Eligibility Verification
We check patients’ insurance coverage before their visit — including plan validity, co-pays, deductibles, and benefits — through payer portals and clearinghouses.

Charge Posting
We post charges into your EMR/billing system from visit notes, ensuring all CPT/ICD-10 codes are captured accurately and tied to each patient encounter.
Payment Posting
We process Electronic Remittance Advice (ERA) and Explanation of Benefits (EOB) to update payment records quickly and accurately in your system.

Electronic Claims Submission
We create, review, and submit claims electronically through clearinghouses, ensuring they’re properly formatted and submitted on time.

Claim Scrubbing
We thoroughly review and clean up claims before submission — checking for missing modifiers, incorrect coding, or NPI mismatches.

Denial Management
We analyse claim denials, correct the root cause (coding, eligibility, submission error), and resubmit them within payer deadlines.

Accounts Receivable (AR) Follow-Up
We follow up on unpaid claims with insurance providers, identifying reasons for delay or non-payment, and work to resolve them promptly.
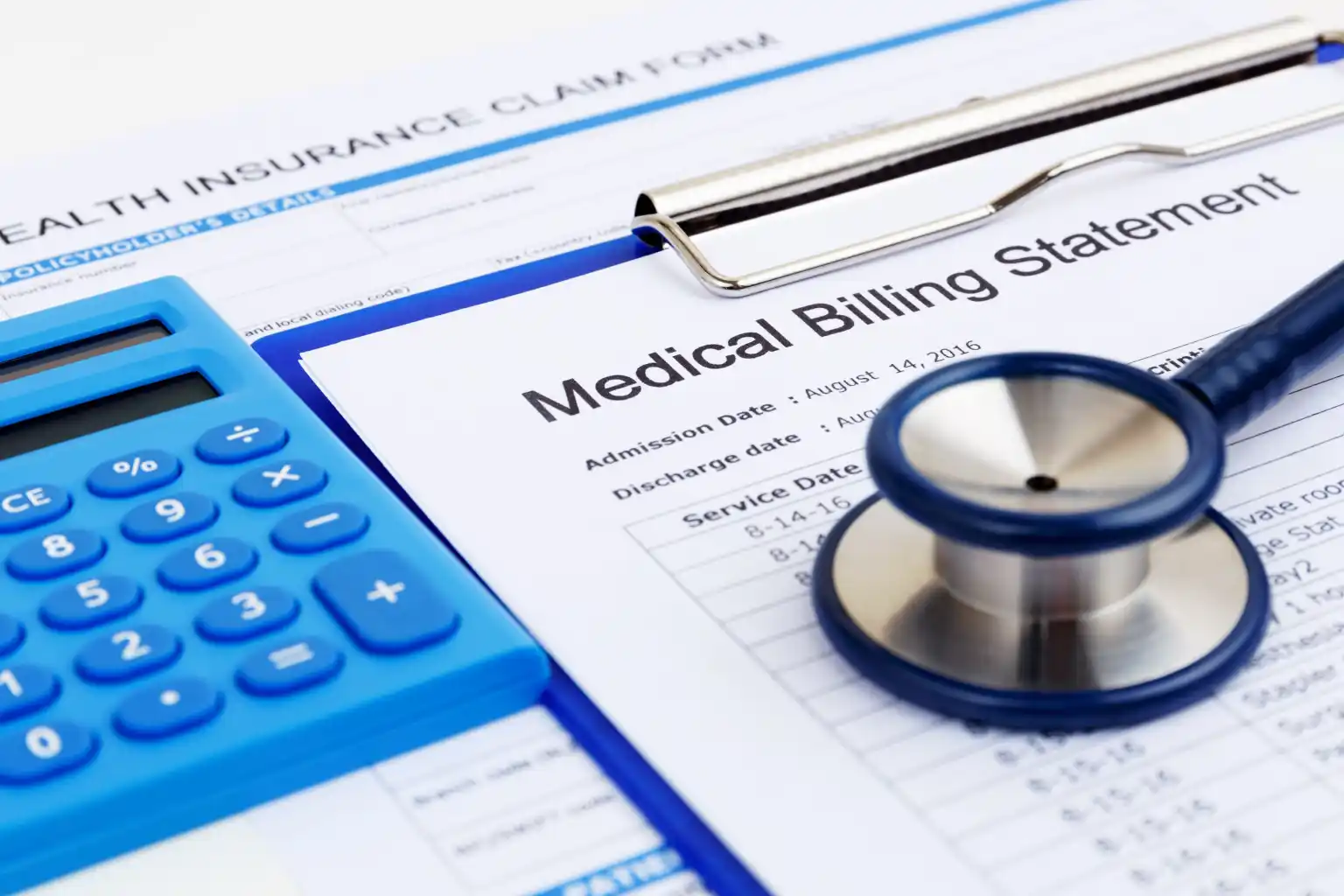
Patient Statements
We generate and send clear, timely billing statements to patients via print or digital methods, including payment support (phone/email).
Testimonials
Experience the Difference, Through Their Eyes
Trusted by clinics, loved by patients.
Join the growing network of U.S. healthcare providers who are saving time and money with MedAxis Global.
Let’s Talk: aaqib@medaxisglobal.com